What is Cardiovascular Disease?
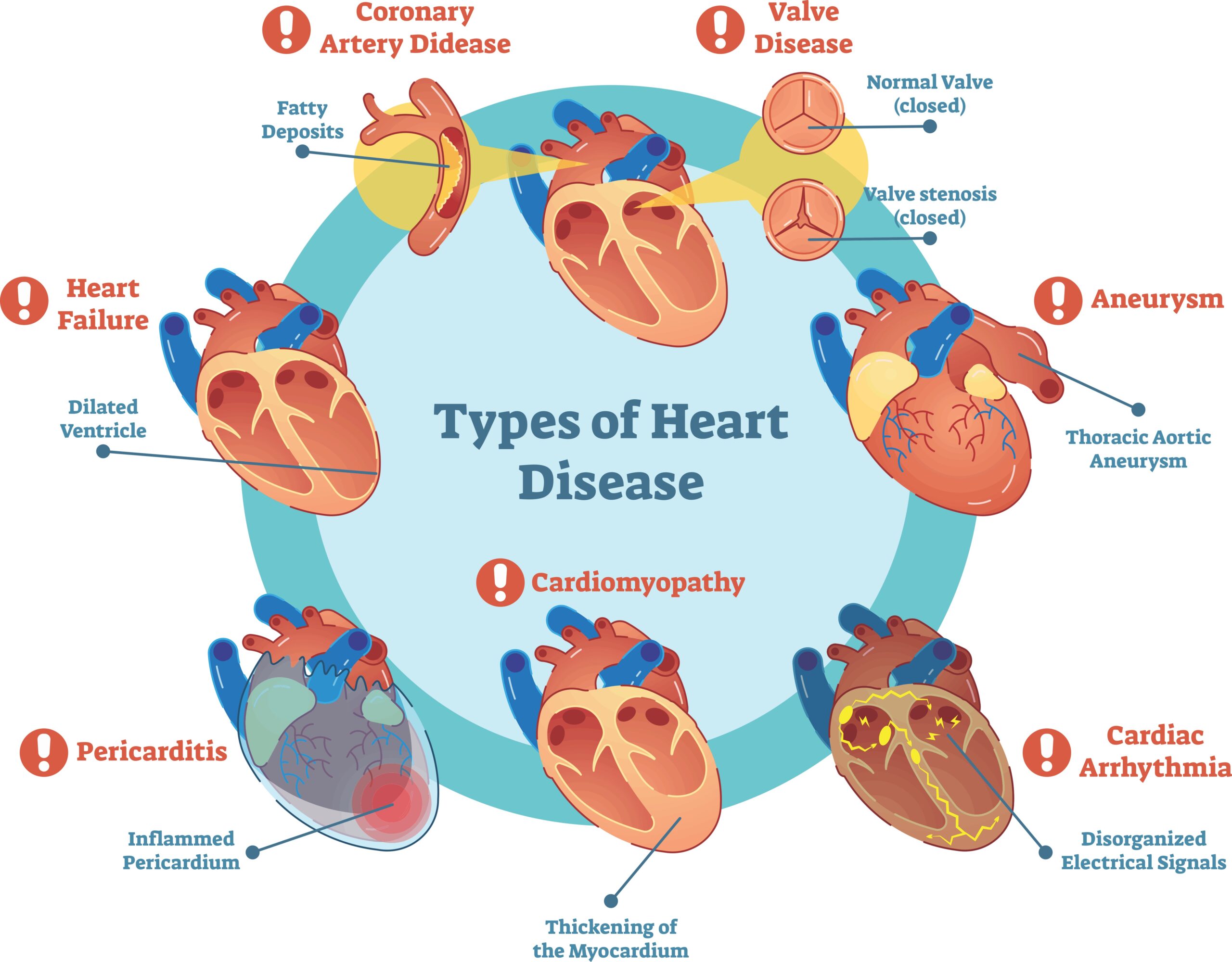
Cardiovascular diseases (CVDs) represent a broad spectrum of conditions affecting the heart and blood vessels.
These include:
- Coronary artery disease (CAD) – narrowing or blockage of arteries supplying the heart.
- Cerebrovascular disease – disorder of the blood vessels supplying the brain, such as stroke and transient ishemic attack (TIA)
- Peripheral arterial disease (PAD) – obstruction of blood flow in arteries outside the heart and brain, usually in the legs.
- Heart failure – the heart’s reduced ability to pump blood effectively.
- Rheumatic and congenital heart disease – due to infection or genetic abnormalities.
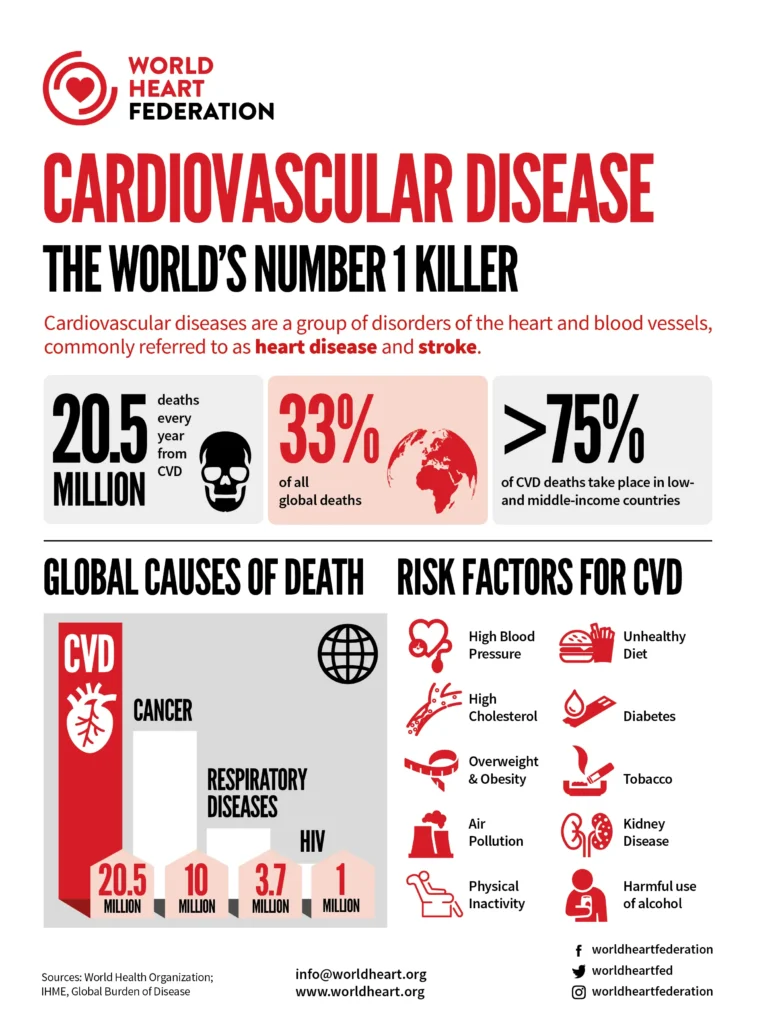
According to the WHO, CVDs are the leading cause of death worldwide, responsible for over 17.9 million deaths per year — that’s 1 in every 3 deaths. Of these, more than 75% occur in low- and middle-income countries. In the UK, CVD causes over 160,000 deaths annually, with an estimated 7.6 million people living with heart or circulatory diseases (British Heart Foundation).
What causes CVDs?
The etiology of CVDs is complex, involving a dynamic interplay between modifiable and non-modifiable risk factors. CVD develops over time through buildup of fatty deposits in the inner walls of arteries.
Modifiable Risk Factors:
- Unhealthy diet
- Physical activity
- Tobacco use
- Excessive alcohol consumption
- Obesity or abdominal fat accumulation
- High blood pressure (hypertension)
- High LDL cholestrol and low HDL cholestrol
- Type 2 Diabetes or insulin resistance
- Chronic stress and poor sleep hygiene
Non-Modifiable Risk Factors:
- Family history of heart disease
- Age – risk increases after 45 for men or 55 for women
- Sex – males are more likely to experience heart disease earlier in life
- Thenicity – e.g. South Asians have higher risk of CAD due to genetic mutation which results in increase in abdominal fat
What are symptoms of CVDs?
The clinical presentation of CVDs is diverse and depends on the specific condition and the extent of the disease.
- Coronary Artery Disease (CAD): Often manifests as angina pectoris (chest pain, tightness, or pressure), typically triggered by physical exertion or emotional stress and relieved by rest or nitroglycerin. Other symptoms can include shortness of breath, fatigue, and palpitations. In women, symptoms can be more atypical, such as nausea, back pain, or jaw pain. A complete blockage of a coronary artery can lead to a myocardial infarction (heart attack), characterized by severe, prolonged chest pain, often radiating to the arm, neck, or jaw, accompanied by sweating, nausea, and shortness of breath.
- Cerebrovascular Disease (Stroke): Occurs when blood flow to a part of the brain is interrupted. Symptoms depend on the area of the brain affected and can include sudden numbness or weakness of the face, arm, or leg (usually on one side of the body), trouble speaking and understanding, vision problems, dizziness, loss of balance, and severe headache. Transient ischemic attacks (TIAs) are “mini-strokes” with temporary symptoms.
- Peripheral Artery Disease (PAD): Affects blood vessels outside the heart and brain, most commonly in the legs. Symptoms include claudication (leg pain during exercise relieved by rest), numbness, coldness, and in severe cases, pain at rest, non-healing sores, and gangrene.
- Heart Failure: A condition where the heart can’t pump enough blood to meet the body’s needs. Symptoms include shortness of breath, fatigue, swelling in the ankles and legs, and rapid or irregular heartbeat.
How can you diagnose CVDs?
A comprehensive diagnostic approach is used to identify CVDs and assess an individual’s risk.
- Clinical Assessment: Includes a thorough medical history, focusing on symptoms, risk factors, and family history, along with a physical examination to check blood pressure, heart rate, and listen for heart murmurs or other abnormalities.
- Electrocardiogram (ECG or EKG): Records the electrical activity of the heart and can detect arrhythmias, signs of ischemia (reduced blood flow), or previous heart attacks.
- Echocardiogram: Uses ultrasound waves to create moving images of the heart, allowing assessment of its structure, function, and valve activity.
- Blood Tests: Measure levels of cholesterol, triglycerides, blood glucose, and cardiac biomarkers (e.g., troponin in cases of suspected heart attack). Inflammatory markers like C-reactive protein (CRP) may also be assessed.
- Exercise Stress Test: Monitors the heart’s electrical activity, blood pressure, and symptoms while the patient exercises on a treadmill or stationary bike, helping to detect ischemia.
- Cardiac Catheterization and Angiography: A thin, flexible tube (catheter) is inserted into a blood vessel and guided to the heart. A contrast dye is injected, and X-rays (angiography) are taken to visualize the coronary arteries and identify blockages.
- Imaging Techniques: Chest X-rays can show the size and shape of the heart and lungs. CT scans and MRI can provide more detailed images of the heart and blood vessels.
Dietary management of CVDs:
Nutrition plays a foundational role in preventing and even reversing early-stage CVD. Evidence strongly supports dietary patterns like Mediterranean diet, DASH diet and plant-forward diets for cardioprotection.
🥦 Core Nutritional Recommendations
- Increase: Leafy greens, berries, legumes, nuts, seeds, oily fish, olive oil, whole grains, garlic
- Limit: Red/processed meats, refined sugars, fried foods, salt, processed carbs, trans fats

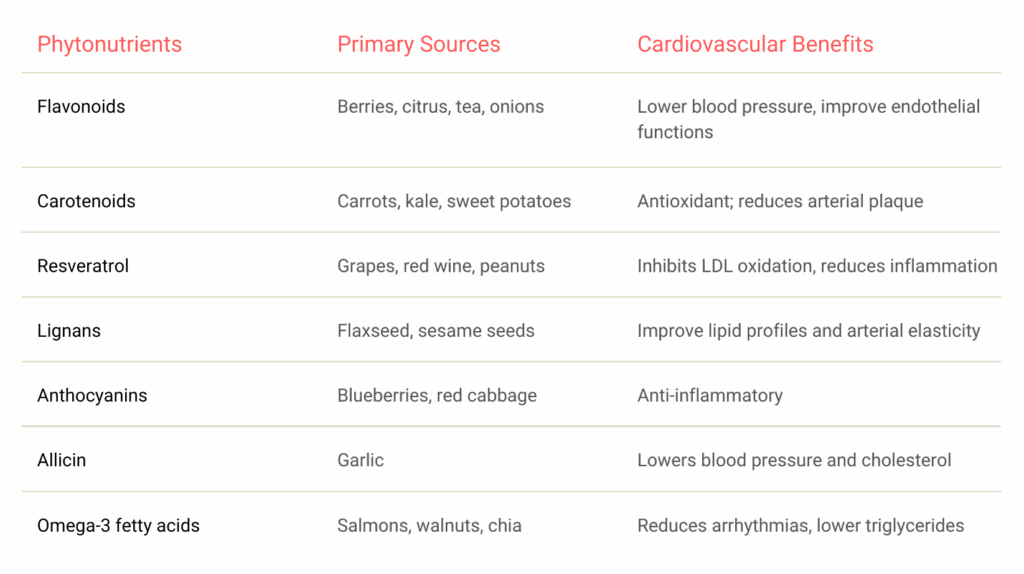
Helpful Phytonutrients for CVDs:
Final Thoughts
Cardiovascular disease may be the world’s leading cause of death — but it is also one of the most preventable. Through evidence-based lifestyle changes, particularly around nutrition, movement, and stress management, individuals can dramatically reduce their risk and even reverse early disease progression. The key lies in consistency, personalisation, and data-driven decision-making — and this is precisely where GastonAI makes a difference. By translating complex health data into everyday food and lifestyle choices, GastonAI empowers individuals to take control of their heart health in real time. In a world where generic advice often falls short, precision nutrition is not just a trend — it’s the future of cardiovascular prevention.






